Getting practical with wearables
As digital data becomes more available and accessible, life insurers are exploring how to
use this alternative data to assess applicants. Risk assessment, which continuously evolves
over time, now has the potential to move to the next level with the arrival of this alternative
data ‒ which is usually easier to access and can enhance the underwriting journey.
However, different is not always better and it is important to understand and test the use
of alternative data.
Using physical activity as an example of alternative data, we dive into five different
applications of alternative data within the life insurance market. We explore how physical
activity data can prove to be successful when used either to augment the existing
underwriting journey or when used on an ongoing basis such as for dynamic underwriting,
resulting in improved accuracy of mortality rates and enhanced predictive power. However,
it is less successful when used to replace or substitute existing underwriting information
since omitting information can lead to reduced predictive power. A possible future
approach is to use physical activity data to personalise the customer journey for applicants
in a way which can result in increased conversion and sales rates.
Lastly, when using alternative data, it is important to do so first in a test and learn
environment with defined goals and criteria. Legal and regulatory considerations are also
essential to any use of alternative data.

Introduction
Underwriting has always involved practical information gathering between the insurance
company and the applicant. The insurer typically wants to know as much as possible about
the risk profile of the applicant while not jeopardising the opportunity to convert a sale.
Historically, this underwriting process has focused on a combination of self-reported
questions, medical reports, and medical tests. However, in recent years, digital data such
as wearable and smartphone data have become more prevalent and easier to access.
Consumers also want to engage more and be recognised (or rewarded) for their lifestyle
which may improve their health management. As a result, life and health insurance
underwriters are contemplating how to use this alternative data to risk-assess applicants.
This paper will focus on how to apply use lifestyle risk factors with a specific focus on
physical activity. It will also run through some real-life case studies and results where
insurance companies are using physical activity in underwriting.
Physical activity
Physical activity is probably the most common health metric which is being monitored and
tracked by people on a regular basis today. It has been shown in many studies to improve
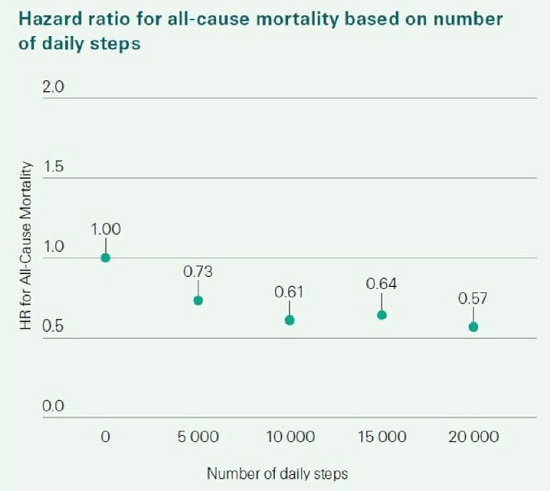
health with better mortality and morbidity outcomes. The recent collaboration between
Swiss Re and Oxford University, using UK Biobank data, confirms this. Because of this
health effect, and the ubiquitous availability of physical activity data (particularly steps),
insurance companies are looking to use it in risk assessment.
Evidence of steps based on a research study collaboration between Swiss Re and Oxford
University:
Although steps data is typically easy to track and is recorded by almost all smartphones
and by all wearables, it is however limited in its tracking of a person’s total physical activity
as it ignores all other types of physical activities. Total physical activity instead consists of
many different activities such as running, walking, climbing stairs, swimming, cycling, etc.
It would be preferable, though not compulsory to track all of a person’s physical activities.
To be able to compare physical activity across these different activities the
metric Metabolic Equivalent of Task (METs) is typically used. METs represents the amount
of energy that you expend when doing an activity compared to that when at rest, whereby
rest is considered to be equivalent to 1 MET. METs are calculated using the intensity,
frequency, and the duration of activities allowing for comparison between different types
of activities. This paper will focus on the use of METs. To put it in perspective, walking at
an average pace (i.e., doing steps) has a MET value of 3, average speed cycling has a MET
value of 6, and average speed running has a MET value of 8. Therefore, five 30-minute
sessions of each activity per week will accumulate to different total physical activity
MET/hours per week of: 7.5 for walking, 15 for cycling and 20 for running.
Why the desire to use wearable data in risk assessment?
Risk assessment has developed and improved over time as more and more health data has
become accessible. Ubiquitous wearable and smartphone data has accelerated the focus
on digital risk assessment. This has primarily been driven by a desire to either get a more
complete picture of a person’s health and thereby offer more competitive premium rates,
or to shorten the risk assessment process and provide customers with a less onerous
onboarding journey.
Physical activity along with the other lifestyle risk factors are now being used to improve
the risk assessment process. Their availability is also creating opportunities for life and
health insurers to engage with consumers in new ways, simplify the onboarding and
underwriting journey, and offer improved tailored propositions. The hope is that this will
lead to improved new business volumes, higher conversion rates and lower lapses.
Insurance companies are eager to explore this data as they recognise that it has the
potential to benefit all parts of the value chain from:
· consumers who have increased health awareness and tracking of their activities
and thereby want to be rewarded through receiving more personalised experiences
· insurers who want to create attractive product propositions and improve their risk
assessment, are seeing the explosion of health apps, wearables, e.g., the Apple
Health kit, as well as the proliferation of credible data, as an opportunity to do this
· society who could reap the benefits of improved health awareness, better wellness,
and reduced global burden of disease
· brokers and advisers who may be able to offer quicker, tech-enabled, and cheaper
insurance offerings to consumers
Key considerations in understanding the value of alternative
data
While there is a large amount of excitement around using wearable data to innovate
underwriting, to unleash the full potential of this alternative data and use it meaningfully is
not as simple as it may seem. It is important to understand the validity and protective value
of this alternative data relative to established practices. We also need to consider how to
interpret this data in a fair and responsible way.
Key to assessing any alternative data in risk assessment is analysing its potential to
provide enhanced commercial value.
Some key considerations with the new data are:
· Is it quicker to access, allowing for greater automation and faster processing?
· Is it cheaper to implement and run?
· Can it provide greater accuracy or predictive value?
· Is it easy to use and based on data or technology that is widely available?
These questions may appear straightforward but many self declared "underwriting
innovations" struggle to answer yes to all of these considerations. Some may offer
incremental increases in speed or accuracy, but come with increased costs due to
increased risks. These questions need to all be considered together to assess the overall
business case for using the alternative data.
Using physical activity data from wearables as an example:
five applications
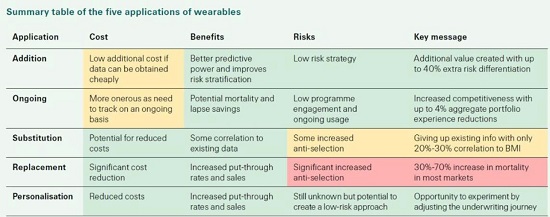
There are five common applications where we, at Swiss Re, see wearable data being
deployed. These applications occur across different risk factors; however, this paper will
focus on physical activity (measured in METs).
The five applications of physical activity data are as follows:
1. Addition: Augmenting current risk assessment with METs to better stratify risk
2. Ongoing/Continuous: Using METs for dynamic underwriting
3. Substitution: 1-for-1 risk factor replacement, e.g., replacing BMI with METs
4. Replacement: METs used in place of several health risk factors
5. Personalisation: Using METs to pre-select customers for different UW journeys
Addition: Is it worth adding METs into the risk assessment
journey?
Our internal research shows that METs have been shown to provide additional predictive
power and risk prediction due to their correlation with better mortality and morbidity
outcomes. This in turn helps to improve risk stratification and has the potential to select
and attract more physically active applicants. The selection is beneficial as it results in an
insurer having a portfolio of policyholders who on average have lower mortality rates, and
this typically allows them to offer more competitive premiums in the market through this
additional risk differentiation.
However, the value of METs also depends on several other factors such as the length and
accuracy of the data as well as the baseline starting MET levels of the group of customers.
If the group of customers has a high starting baseline level of METs, this will reduce the
potential for mortality improvements.
When expanding this to other risk factors, the level of underwriting risk differentiation can
be significantly enhanced. The graph below, based on our internal research on a mortality
risk pool, illustrates the potential to increase the range of risk differentiation when adding
several lifestyle risk factors into risk assessment. It compares this range under two
scenarios: 1) when only using clinical factors and 2) when using both clinical and lifestyle
factors. The range is calculated by looking at the minimum and maximum range of each
risk factor whereby each one individually would still place the person in a standard
underwriting pool.
Under the first scenario when only using clinical factors such as (BMI, blood pressure,
cholesterol and HBA1C), the range of risk differentiation is 122% (from -39% to 83%). This
range increases on both sides to 201% (from -55% to 146%) under the second scenario,
when also including lifestyle risk factors such as physical activity, nutrition, sleep, and
mental wellness.
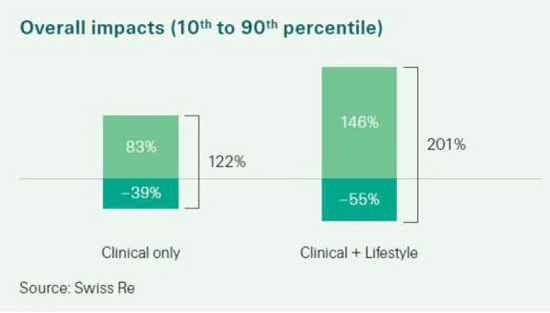
It is important to note that a wider risk differentiation range does not mean that a portfolio
will suddenly have better mortality rates.
It is still a zero-sum game whereby the consumers who receive additional discounts for a
healthy lifestyle should be balanced against less healthy lives who may receive additional
loadings. Insurers will therefore need to create additional value by attracting healthier lives
through the additional risk stratification and thereby generate better mortality rates.
One of the additional goals of engaging with consumers by using wearable or lifestyle data,
is the potential to help policyholders improve both their health and insurability by using
linked wellness and lifestyle programs. This should however, the benefits of additional risk
differentiation (e.g. the potential to positively select healthier applicants) need to be
considered against the costs and ease of obtaining this data on a one-off basis, as well as
the credibility of the data, the robustness of the historical data, and other competitive
pressures.
Ongoing: Is there a future for dynamic underwriting?
Dynamic underwriting has gained attention in recent years, even before the explosion of
wearables. The idea of policyholders engaging with and improving their clinically
modifiable risk factors (e.g., BMI or blood pressure) to gain some financial or other reward
benefit, has been around for over a decade.
Wearables promise a more automated and consistent flow of information to update
modifiable lifestyle risk. METs have been shown to be an excellent fit for dynamic
underwriting; the data is widely available and easy to access. Over the medium to longterm,
the predictive power of tracking METs makes it easier to identify, price for, and drive
healthy behaviour change which can help to reduce a customer’s risk or prevent their risk
worsening. METs can also be used to promote policyholder wellbeing on an ongoing basis,
allowing insurers to incentivise and reward positive behaviour.
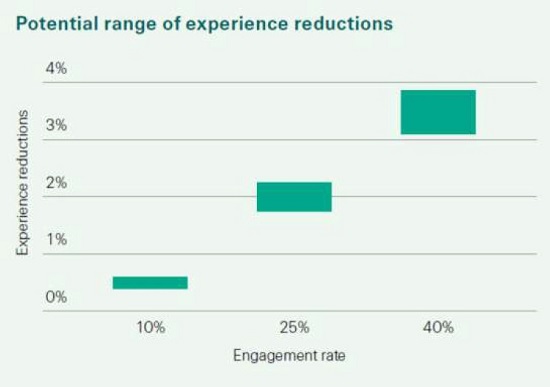
Our global internal data research shows that health and wellness engagement platforms
that track and reward particular levels of METs, as well as run annual health assessments
that track other clinical and lifestyle risk factors may be able to see aggregate mortality and
lapse experience reductions of up to 4% across the entire insurance policy book, with a
substantial proportion of the benefit coming from getting customers to positively change
their behaviours. This is shown in the graph below.
Substitution: Can METs be a 1-1 risk factor replacement?
Although METs as a risk factor has some protective value, research shows that it cannot
simply replace existing underwriting risk factors. If we were to replace BMI with METs,
data shows that this approach could lead to important and meaningful gaps in risk
assessment. In fact, the US National Health and Nutrition Examination Survey (NHANES)
database and UK Biobank both show low overall correlation, as is shown in the graphs
below:
· < 30% on NHANES between BMI and METS even after allowing for diseases
· 20% on the UK Biobank between BMI and step count when using accelerometer
data.
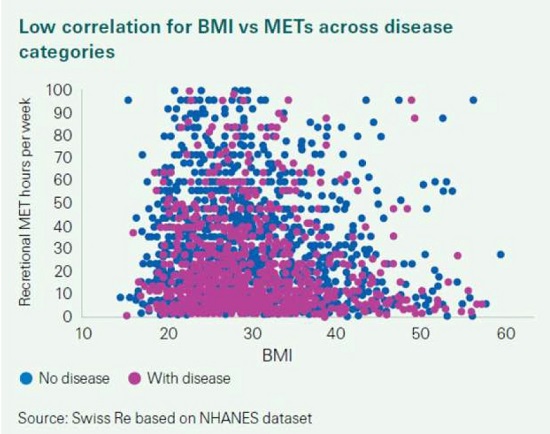
As a result, replacing BMI or steps with METs could result in lives with higher BMI levels
selecting into the product. The level of anti-selection will though depend on factors such as
competitive considerations, relevant market disclosure rates, target audience (e.g., age)
and the range of BMI values.
There are certain situations where insurance companies would typically be more
supportive of a substitution approach, e.g., where several mitigants or pre-selection may
exist, such as people who are originally part of a wellness program, or young athletes. Also,
in a market with poor BMI disclosure, using more objective wearable METs may actually
help to improve risk selection.
Replacement: Can METs completely replace traditional clinical
risk factors and medical history – are we ready?
Some InsurTech companies promote a view that METs alone are as predictive as current
underwriting. The view is that by collecting METs, age, gender and only a couple of other
risk factors, they can create a portfolio that in some circumstances is at least 95% as
predictive as current underwriting and hence a shorter underwriting approach could be
adopted.
Although the frequency of inaccuracy can be low, the severity of the incorrectly priced risks
can be very high. As an example, the NHANES data shows that there is a low correlation
between people having a disease and METs (< 20%) as shown in the graph below. This
means that underwriting that relies solely only METs, will result in people with medical
diseases being added into the standard underwriting pool without being priced correctly.
The potential for anti-selection can also increase significantly if diseases are not being
considered. In fact, our internal data research shows that this anti-selection increases
claims costs by as much as 30-70% in most markets and rises to a 100% or more in
markets which offer preferred products.
Legal and regulatory considerations
Legal and regulatory attention is growing when it comes to using alternative data in risk
assessment and algorithmic underwriting approaches. Therefore, it is paramount to
consider these aspects.
Some specific challenges include:
· how to treat customers fairly in pricing, underwriting, and product structure with
the alternative data and ensure equitable risk selection for those that do not have
such data available
· whether the use of the alternative data creates any unfair discrimination, e.g.,
across ages, income status based on access to wearable devices, ethnicity, etc.
· bias due to data collection opportunities
· lack of transparency in “black box” risk selection algorithms
· use and transfer of personal data for risk selection purposes
· how non-disclosure or misrepresentation might work in a world of alternative
underwriting data and the ability of insurers to challenge misrepresented or
erroneous data (i.e. in wearables)
· how best to encourage of customers to use wearable apps and share their data
· how to inform and get consent from applicants to use the data in risk assessment
· ensuring data privacy considerations
· not create disadvantages for certain segments of society who do not have access to
wearable devices, e.g., due to affordability



